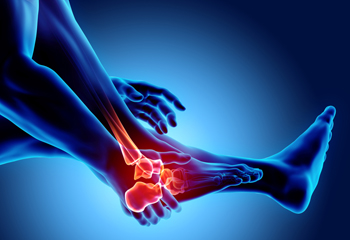
 Experiencing heel pain can significantly impact your daily life, making even simple tasks like walking or standing uncomfortable. Podiatrists, medical professionals specializing in foot and ankle health, can diagnose and treat heel pain. These types of doctors understand the complex structure of the foot and can identify the underlying causes of heel pain. Included are overuse injuries like plantar fasciitis, bone spurs, or Achilles tendonitis. Targeting the underlying cause of heel pain is important for appropriate care. It is especially important to seek the advice of a podiatrist if you have persistent pain, and if the pain comes suddenly or after an injury. A podiatrist can offer a personalized treatment plan that may include specialized exercises, custom orthotics, medication, or advanced therapies designed to alleviate pain and promote healing. Podiatrists can also provide valuable guidance on footwear choices and lifestyle modifications to prevent future pain. If you are suffering from heel pain, it is suggested you seek the help of a podiatrist for diagnosis and care.
Experiencing heel pain can significantly impact your daily life, making even simple tasks like walking or standing uncomfortable. Podiatrists, medical professionals specializing in foot and ankle health, can diagnose and treat heel pain. These types of doctors understand the complex structure of the foot and can identify the underlying causes of heel pain. Included are overuse injuries like plantar fasciitis, bone spurs, or Achilles tendonitis. Targeting the underlying cause of heel pain is important for appropriate care. It is especially important to seek the advice of a podiatrist if you have persistent pain, and if the pain comes suddenly or after an injury. A podiatrist can offer a personalized treatment plan that may include specialized exercises, custom orthotics, medication, or advanced therapies designed to alleviate pain and promote healing. Podiatrists can also provide valuable guidance on footwear choices and lifestyle modifications to prevent future pain. If you are suffering from heel pain, it is suggested you seek the help of a podiatrist for diagnosis and care.
Many people suffer from bouts of heel pain. For more information, contact Dr. Richard DiMario of Maine. Our doctor can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions please contact our office located in York, ME . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.

The feet can be affected by falling. In older adults, this may lead to them having difficulty in completing daily activities. Ensuring a safe living space for aging loved ones is vital for their well-being and independence. Begin by decluttering walkways and removing tripping hazards such as loose rugs or electrical cords. Install handrails along stairways and in bathrooms to provide stability and support. Secure carpets and rugs with non-slip backing to prevent slips and falls. Improve lighting throughout the home, especially in hallways, staircases, and entrances. Consider installing grab bars and shower chairs in bathrooms, and keep commonly used items within easy reach to avoid the need for reaching or bending over. Additionally, consider investing in assistive devices, such as mobility aids or medical alert systems, for added safety and peace of mind. Regularly assess the home environment for potential hazards, and make necessary adjustments to promote a secure and comfortable living environment for aging loved ones. If you are seeking additional falls prevention methods that can protect the feet, it is suggested that you consult a podiatrist who can offer you valuable information.
Preventing falls among the elderly is very important. If you are older and have fallen or fear that you are prone to falling, consult with Dr. Richard DiMario from Maine. Our doctor will assess your condition and provide you with quality advice and care.
Every 11 seconds, an elderly American is being treated in an emergency room for a fall related injury. Falls are the leading cause of head and hip injuries for those 65 and older. Due to decreases in strength, balance, senses, and lack of awareness, elderly persons are very susceptible to falling. Thankfully, there are a number of things older persons can do to prevent falls.
How to Prevent Falls
Some effective methods that older persons can do to prevent falls include:
Falling can be a traumatic and embarrassing experience for elderly persons; this can make them less willing to leave the house, and less willing to talk to someone about their fears of falling. Doing such things, however, will increase the likelihood of tripping or losing one’s balance. Knowing the causes of falling and how to prevent them is the best way to mitigate the risk of serious injury.
If you have any questions, please feel free to contact our office located in York, ME . We offer the newest diagnostic and treatment technologies for all your foot care needs.

Stretching is not just beneficial for major muscle groups, but also for the often neglected toes, which play a vital role in maintaining balance and stability. Simple yet effective toe stretches can help alleviate discomfort, improve flexibility, and prevent common foot issues. Begin with the toe extension stretch by sitting comfortably and gently pulling each toe back, holding for a few seconds to feel the stretch along the top of the foot. Another beneficial stretch is the toe flexion stretch, where you sit and interlace your fingers between your toes, gently pressing them together to stretch the toe joints. Additionally, the toe spread exercise involves using your fingers to separate and stretch each toe outward, promoting better circulation and flexibility. If you are looking to learn about additional toe and foot stretches, it is suggested that you visit a podiatrist who can provide you with the knowledge you are seeking.
Stretching the feet is a great way to prevent injuries. If you have any concerns with your feet consult with Dr. Richard DiMario from Maine. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Stretching the Feet
Being the backbone of the body, the feet carry your entire weight and can easily become overexerted, causing cramps and pain. As with any body part, stretching your feet can serve many benefits. From increasing flexibility to even providing some pain relief, be sure to give your feet a stretch from time to time. This is especially important for athletes or anyone performing aerobic exercises, but anyone experiencing foot pain or is on their feet constantly should also engage in this practice.
Great ways to stretch your feet:
Individuals who tend to their feet by regular stretching every day should be able to minimize foot pain and prevent new problems from arising.
If you have any questions, please feel free to contact our office located in York, ME . We offer the newest diagnostic and treatment technologies for all your foot care needs.

A podiatrist specializes in treating foot, ankle, and lower limb conditions, providing care for ailments that can include fractures, nerve damage, and sports injuries. These doctors undergo extensive education, including a Doctor of Podiatric Medicine, or DPM, degree and residency training, focusing on lower extremity issues. Podiatrists diagnose and treat various conditions, from structural abnormalities to skin and nail disorders. Some podiatrists specialize in areas like orthotics, diabetes care, or surgery. They use diagnostic tools, such as imaging tests and sensory evaluations, to assess foot health accurately. Treatment options range from medication and injections to corrective footwear and surgery. Podiatrists are essential in managing foot-related issues. If you have a recent foot or ankle injury or are suffering with chronic discomfort in these areas, it is suggested that you schedule an appointment with a podiatrist for a proper diagnosis and treatment options.
If you are experiencing pain in the feet or ankles, don’t join the stubborn majority refusing treatment. Feel free to contact Dr. Richard DiMario from Maine. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Podiatrist?
Someone would seek the care of a podiatrist if they have suffered a foot injury or have common foot ailments such as heal spurs, bunions, arch problems, deformities, ingrown toenails, corns, foot and ankle problems, etc.
Podiatric Treatment
A podiatrist will treat the problematic areas of the feet, ankle or lower leg by prescribing the following:
A common podiatric procedure a podiatrist will use is a scanner or force plate which will allow the podiatrist to know the designs of orthotics. Patients are then told to follow a series of tasks to complete the treatment. The computer will scan the foot a see which areas show weight distribution and pressure points. The podiatrist will read the analysis and then determine which treatment plans are available.
If you have any questions please feel free to contact our office located in York, ME . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.

Athlete's foot, a common fungal infection, affects the skin of the feet and thrives in warm, damp environments such as sweaty socks and communal showers. The primary cause is the fungus trichophyton, which spreads through direct contact with contaminated surfaces or through contact with infected individuals. The signs and symptoms of athlete's foot vary, but often include itching, burning sensations, and redness between the toes or on the soles of the feet. In some cases, blisters or cracked skin may develop, leading to discomfort and pain. If left untreated, athlete's foot can spread to other areas of the body and cause secondary infections. Proper hygiene practices, such as keeping the feet clean and dry, wearing breathable footwear, and avoiding walking barefoot in public areas, may help to prevent athlete's foot. Early recognition and management are key to resolving athlete's foot and preventing its recurrence. If you have any of the above symptoms, it is strongly suggested that you visit a podiatrist as quickly as possible who can provide you with the necessary medication for relief and treatment.
Athlete’s Foot
Athlete’s foot is often an uncomfortable condition to experience. Thankfully, podiatrists specialize in treating athlete’s foot and offer the best treatment options. If you have any questions about athlete’s foot, consult with Dr. Richard DiMario from Maine. Our doctor will assess your condition and provide you with quality treatment.
What Is Athlete’s Foot?
Tinea pedis, more commonly known as athlete’s foot, is a non-serious and common fungal infection of the foot. Athlete’s foot is contagious and can be contracted by touching someone who has it or infected surfaces. The most common places contaminated by it are public showers, locker rooms, and swimming pools. Once contracted, it grows on feet that are left inside moist, dark, and warm shoes and socks.
Prevention
The most effective ways to prevent athlete’s foot include:
Symptoms
Athlete’s foot initially occurs as a rash between the toes. However, if left undiagnosed, it can spread to the sides and bottom of the feet, toenails, and if touched by hand, the hands themselves. Symptoms include:
Diagnosis and Treatment
Diagnosis is quick and easy. Skin samples will be taken and either viewed under a microscope or sent to a lab for testing. Sometimes, a podiatrist can diagnose it based on simply looking at it. Once confirmed, treatment options include oral and topical antifungal medications.
If you have any questions, please feel free to contact our office located in York, ME . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot arthritis, a multifaceted condition, manifests in various ways, each presenting distinct challenges for those grappling with joint inflammation in the feet. Osteoarthritis, the most common form, results from wear and tear on the joints, causing pain and stiffness. Rheumatoid arthritis, an autoimmune disorder, targets the joints and may lead to deformities in the feet. Gout, characterized by the accumulation of uric acid crystals, induces sudden and severe pain. Recognizing the specific type of foot arthritis is essential for implementing targeted relief methods. While medications are common approaches to treatment, lifestyle modifications such as maintaining a healthy weight and choosing supportive footwear can help to alleviate symptoms. Resting the feet and engaging in gentle exercises can provide relief. Foot arthritis can cause discomfort, and if you are suffering from this condition, it is suggested that you visit a podiatrist who can guide you toward effective relief methods.
Arthritis can be a difficult condition to live with. If you are seeking treatment, contact Dr. Richard DiMario from Maine. Our doctor can provide the care you need to keep you pain-free and on your feet.
Arthritic Foot Care
Arthritis is a term that is commonly used to describe joint pain. The condition itself can occur to anyone of any age, race, or gender, and there are over 100 types of it. Nevertheless, arthritis is more commonly found in women compared to men, and it is also more prevalent in those who are overweight. The causes of arthritis vary depending on which type of arthritis you have. Osteoarthritis for example, is often caused by injury, while rheumatoid arthritis is caused by a misdirected immune system.
Symptoms
Arthritic symptoms range in severity, and they may come and go. Some symptoms stay the same for several years but could potentially get worse with time. Severe cases of arthritis can prevent its sufferers from performing daily activities and make walking difficult.
Risk Factors
If you suspect your arthritis is affecting your feet, it is crucial that you see a podiatrist immediately. Your doctor will be able to address your specific case and help you decide which treatment method is best for you.
If you have any questions, please feel free to contact our office located in York, ME . We offer the newest diagnostic and treatment technologies for all your foot care needs.

Proper foot care is essential for anyone with diabetes, as the condition can compromise blood flow and damage nerves. Following these essential steps for diabetic foot care can help a diabetic patient prevent other serious health issues. Start by washing your feet daily with warm water and mild soap, ensuring thorough drying and the application of lotion, excluding the spaces between toes to prevent infections. A daily visual inspection is extremely important to identify potential problems early, given the reduced sensation and circulation associated with diabetes. Trim toenails straight across to prevent ingrown nails, taking special care to avoid cutting cuticles. Choose comfortable footwear, steering clear of high heels and pointy toes, and consider custom orthotics for added support. Protect your feet from injuries by avoiding walking barefoot, wearing quality socks, and refraining from using sharp tools for corn and callus removal. Additionally, manage blood sugar levels and quit smoking to reduce the risk of complications. Many people with diabetes also suffer from neuropathy and peripheral artery disease, which can result in foot ulcers. For this reason, it is suggested that you schedule regular visits with a podiatrist who is medically trained to manage the side effects of this disease.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact Dr. Richard DiMario from Maine. Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our office located in York, ME . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.

Foot fractures are common injuries that podiatrists frequently encounter, often involving the metatarsals and toes. Patients typically exhibit various symptoms, with pain and difficulty while walking being the most prevalent. Diagnosis relies on radiographic assessment or ultrasonography. The choice of management depends on the fracture's location and its impact on balance and weight-bearing. Treatment options may include splinting, avoiding weight-bearing activities, casts, boots, or orthotics. If you have sustained a foot fracture of any type, it is suggested that you schedule an appointment with a podiatrist for a proper evaluation and relief options
A broken foot requires immediate medical attention and treatment. If you need your feet checked, contact Dr. Richard DiMario from Maine. Our doctor can provide the care you need to keep you pain-free and on your feet.
Broken Foot Causes, Symptoms, and Treatment
A broken foot is caused by one of the bones in the foot typically breaking when bended, crushed, or stretched beyond its natural capabilities. Usually the location of the fracture indicates how the break occurred, whether it was through an object, fall, or any other type of injury.
Common Symptoms of Broken Feet:
Those that suspect they have a broken foot shoot seek urgent medical attention where a medical professional could diagnose the severity.
Treatment for broken bones varies depending on the cause, severity and location. Some will require the use of splints, casts or crutches while others could even involve surgery to repair the broken bones. Personal care includes the use of ice and keeping the foot stabilized and elevated.
If you have any questions please feel free to contact our office located in York, ME . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.