
Blood blisters on the foot are caused by friction or trauma that ruptures blood vessels under the skin without breaking the surface. This can occur from wearing ill-fitting shoes, engaging in vigorous activities, or sudden impact injuries. The resulting blister is filled with blood due to the broken capillaries beneath the skin. Blood blisters are generally more painful than regular blisters because of the pressure from the trapped blood. They typically last for about one to two weeks, during which time the body gradually reabsorbs the blood. To aid healing, it is important to protect the blister from further friction or pressure by using padded bandages and avoiding activities that aggravate the area. If you notice you have a blood blister on your foot, it is suggested that you schedule an appointment with a podiatrist who can help you to manage this condition.
Blisters are prone to making everyday activities extremely uncomfortable. If your feet are hurting, contact Dr. Richard DiMario of Maine. Our doctor can provide the care you need to keep you pain-free and on your feet.
Foot Blisters
Foot blisters develop as a result of constantly wearing tight or ill-fitting footwear. This happens due to the constant rubbing from the shoe, which can often lead to pain.
What Are Foot Blisters?
A foot blister is a small fluid-filled pocket that forms on the upper-most layer of the skin. Blisters are filled with clear fluid and can lead to blood drainage or pus if the area becomes infected.
How Do Blisters Form?
Blisters on the feet are often the result of constant friction of skin and material, usually by shoe rubbing. Walking in sandals, boots, or shoes that don’t fit properly for long periods of time can result in a blister. Having consistent foot moisture and humidity can easily lead to blister formation.
Prevention & Treatment
It is important to properly care for the affected area in order to prevent infection and ease the pain. Do not lance the blister and use a Band-Aid to provide pain relief. Also, be sure to keep your feet dry and wear proper fitting shoes. If you see blood or pus in a blister, seek assistance from a podiatrist.
If you have any questions, please feel free to contact our office located in York, ME . We offer the newest diagnostic and treatment technologies for all your foot care needs.

Foot ulcers are open wounds that develop on the feet, often affecting individuals with diabetes or impaired circulation. They typically occur due to a combination of factors, including neuropathy, which is nerve damage, poor blood flow, and pressure from footwear. Foot ulcers can vary in severity, from shallow sores to deep craters, and if left untreated, they can lead to serious complications such as infection and possibly amputation. The primary cause of foot ulcers is prolonged pressure or friction on the skin, which can result from wearing ill-fitting shoes, walking barefoot, or excessive rubbing. In diabetic individuals, high blood sugar levels can further exacerbate the risk by damaging nerves and blood vessels, impairing the body's ability to heal. Other contributing factors may include poor hygiene, smoking, obesity, and a history of foot problems. Recognizing the signs of a foot ulcer, such as redness, swelling, or drainage, is vital for prompt treatment and prevention of complications. If you have a foot wound, it is strongly suggested that you consult a podiatrist who can diagnose its severity, and offer treatment options that are right for you.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Dr. Richard DiMario from Maine. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in York, ME . We offer the newest diagnostic and treatment technologies for all your foot care needs.

A bunion, medically termed hallux valgus, is a bony protrusion on the inner side of the foot, precisely at the base of the big toe. This condition arises from the misalignment of the bones in the forefoot, compelling the big toe to angle towards the lesser toes, consequently protruding the joint at its base. Bunions can cause significant discomfort and interfere with your daily activities. If you have exhausted nonsurgical options like padding or orthotic shoes, bunion surgery may be the next step to relieve your pain and improve mobility. During the procedure, a podiatrist may remove the bunion, realign bones, or release tight ligaments to straighten your big toe. Risks of bunion surgery include nerve damage, bone healing issues, or overcorrection. The recovery process often takes up to six months. Initially, you may need to keep your leg elevated to reduce swelling, and it can take weeks before you can comfortably wear regular shoes again. Among the long-term benefits of bunion surgery are improved comfort and mobility. If you are struggling with bunion pain, it is suggested that you consult a podiatrist to discuss whether surgery is right for you.
If you are suffering from bunions, contact Dr. Richard DiMario of Maine. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
If you have any questions, please feel free to contact our office located in York, ME . We offer the newest diagnostic and treatment technologies for all your foot care needs.
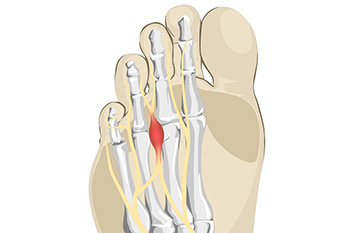
Morton's neuroma, named after the American surgeon Thomas G. Morton who first described it in the 19th century, is a painful condition affecting the nerves in the foot. This benign growth typically forms between the third and fourth toes, resulting from compression or irritation of the interdigital nerve. The exact cause of Morton's neuroma remains elusive, but factors such as wearing tight or high-heeled shoes, engaging in repetitive high-impact activities, or foot deformities may contribute to its development. Symptoms of Morton's neuroma often include a sharp, burning pain or sensation of a lump or foreign object in the ball of the foot. Individuals may also experience numbness, tingling, or a feeling of walking on a pebble. As the condition progresses, discomfort may worsen and become more persistent, particularly during weight-bearing activities. If you have pain in this part of your foot, it may be Morton's neuroma, and it is suggested that you visit a podiatrist. This type of doctor can accurately diagnose and effectively treat this condition.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Dr. Richard DiMario of Maine. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our office located in York, ME . We offer the newest diagnostic and treatment technologies for all your foot care needs.