
Athlete’s foot is a fungal infection that affects the skin on the feet, causing itching, burning, and peeling. It is caused by dermatophytes, a type of fungus that thrives in warm, moist environments like locker rooms, swimming pools, and public showers. The infection spreads through direct contact or by sharing contaminated items such as towels or shoes. Those who sweat excessively or wear tight, non-breathable shoes are at higher risk. Symptoms of athlete’s foot include red, scaly skin, blisters, and cracked skin, often between the toes or on the soles of the feet. If left untreated, the infection can spread to other areas of the body, including the nails or groin, and may lead to bacterial infections. Persistent infections may require stronger medications or specialized care. A podiatrist can accurately diagnose the condition and recommend the best treatment plan. If you are experiencing symptoms of athlete’s foot, it is suggested that you schedule an appointment with a podiatrist.
Athlete’s foot is an inconvenient condition that can be easily reduced with the proper treatment. If you have any concerns about your feet and ankles, contact Dr. Richard DiMario from Maine. Our doctor will treat your foot and ankle needs.
Athlete’s Foot: The Sole Story
Athlete's foot, also known as tinea pedis, can be an extremely contagious foot infection. It is commonly contracted in public changing areas and bathrooms, dormitory style living quarters, around locker rooms and public swimming pools, or anywhere your feet often come into contact with other people.
Solutions to Combat Athlete’s Foot
Athlete’s foot can cause many irritating symptoms such as dry and flaking skin, itching, and redness. Some more severe symptoms can include bleeding and cracked skin, intense itching and burning, and even pain when walking. In the worst cases, Athlete’s foot can cause blistering as well. Speak to your podiatrist for a better understanding of the different causes of Athlete’s foot, as well as help in determining which treatment options are best for you.
If you have any questions please feel free to contact our office located in York, ME . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
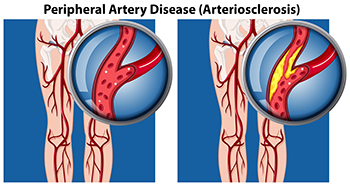
Peripheral artery disease, known as PAD, occurs when the blood vessels in the legs and feet become narrowed or blocked, reducing blood flow. This leads to symptoms like leg pain, cramping, or fatigue, particularly when walking or exercising. PAD can also cause sores or ulcers that are slow to heal, or cold, pale feet. In severe cases, it can increase the risk of infections or even amputation, if left untreated. The primary cause of PAD is atherosclerosis, a condition where fatty deposits build up in the arteries. Risk factors include smoking, diabetes, high blood pressure, and high cholesterol. Treatment for PAD often involves lifestyle changes, such as quitting smoking, exercising, and managing blood sugar and cholesterol levels. Medications or surgery may be necessary in more advanced cases. A podiatrist can assess your condition, provide effective treatments, and help prevent complications. If you are experiencing symptoms of PAD, it is suggested that you schedule an appointment with a podiatrist.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with Dr. Richard DiMario from Maine. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our office located in York, ME . We offer the newest diagnostic and treatment technologies for all your foot care needs.

Nighttime gout flares often cause intense pain, swelling, and redness in the feet, and can severely disrupt sleep. Gout is a form of arthritis caused by a buildup of uric acid in the joints, and it frequently affects the big toe due to its susceptibility to stress and lower temperatures. Nighttime gout attacks may be linked to factors such as dehydration, reduced body temperature, and lower cortisol levels during sleep. These painful episodes can make it difficult for patients to find relief without medical help. A podiatrist can assess symptoms, confirm a diagnosis, and recommend strategies to reduce the frequency and severity of gout flares. These may include lifestyle modifications such as changes in diet, preventative techniques like weight loss, and treatments to alleviate pain and inflammation in the affected joints. Proper management not only helps to protect the health of your feet and ankles but also improves sleep patterns. If you have nighttime flare-ups of gout, it is suggested that you schedule an appointment with a podiatrist for guidance in managing this painful condition.
Gout is a painful condition that can be treated. If you are seeking treatment, contact Dr. Richard DiMario from Maine. Our doctor will treat your foot and ankle needs.
What Is Gout?
Gout is a form of arthritis that is characterized by sudden, severe attacks of pain, redness, and tenderness in the joints. The condition usually affects the joint at the base of the big toe. A gout attack can occur at any random time, such as the middle of the night while you are asleep.
Symptoms
Risk Factors
Prior to visiting your podiatrist to receive treatment for gout, there are a few things you should do beforehand. If you have gout you should write down your symptoms--including when they started and how often you experience them, important medical information you may have, and any questions you may have. Writing down these three things will help your podiatrist in assessing your specific situation so that he or she may provide the best route of treatment for you.
If you have any questions, please feel free to contact our office located in York, ME . We offer the newest diagnostic and treatment technologies for all your foot care needs.

A bunion is a bony bump that forms at the base of the big toe, where it angles toward the second toe. This condition occurs when the bones in the front of the foot shift out of alignment, causing the big toe to lean inward. Over time, the misalignment leads to the formation of a prominent bump on the joint. Symptoms of bunions include pain, swelling, redness, and the development of calluses or corns where the toes rub against the shoe. The pain can worsen with prolonged standing or walking. Common causes of bunions include genetics, wearing tight or ill-fitting shoes, and excessive pressure on the feet. Conditions like arthritis or flat feet can also contribute to the development of bunions. While bunions may be managed with conservative treatments, surgery may be needed for severe cases to restore normal foot function and alleviate pain. If you have symptoms of a bunion, it is suggested that you consult a podiatrist who can guide you toward treatment methods that are right for you.
If you are suffering from bunions, contact Dr. Richard DiMario of Maine. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
If you have any questions, please feel free to contact our office located in York, ME . We offer the newest diagnostic and treatment technologies for all your foot care needs.

Plantar fibromas are benign growths of fibrous tissue that develop within the plantar fascia, the thick band of tissue running along the sole of the foot. These firm nodules are often found in the arch and may cause discomfort, especially when walking or standing. The exact cause is unknown, but plantar fibromas may develop due to genetic predisposition, minor injuries, or repetitive stress on the foot. People with a family history or those with certain medical conditions, such as diabetes or liver disease, are more likely to experience them. Diagnosis involves a physical examination by a podiatrist, who may confirm the presence of fibromas with imaging tests like an ultrasound or MRI scans. Treatment options include custom orthotic inserts, corticosteroid injections, targeted exercises, and in severe cases, surgical removal. If you have symptoms of plantar fibroma, it is suggested that you schedule an appointment with a podiatrist for a proper diagnosis and treatment.
A plantar fibroma may disrupt your daily activities. If you have any concerns, contact Dr. Richard DiMario of Maine. Our doctor can provide the care you need to keep you pain-free and on your feet.
Plantar Fibroma
A plantar fibroma is a fibrous knot in the arch of the foot. It is embedded in the plantar fascia which is a band of tissue that extends from the heel to the toes along the bottom of the foot. There can be multiple plantar fibromas in the feet at the same time. There are no known causes for this condition. If you have a plantar fibroma, there will be a bump in the arch of your foot that cannot be missed. Any associated pain is most often due to a shoe rubbing against the nodule. Non-surgical options, such as steroid injections, physical therapy, and orthotics should be tried first. Surgery is a last resort and is the only thing that will remove a plantar fibroma entirely. Consult with a podiatrist for a proper diagnosis and to determine the treatment regimen that is right for you.
What Causes a Plantar Fibroma?
While there are no specific causes identified, a plantar fibroma can possibly come from genetic predisposition or the formation of scar tissue that forms from healing the tears in the plantar fascia.
What Are the Symptoms of a Plantar Fibroma?
There will be a noticeable lump in the arch of the foot that may or may not cause pain. If pain is felt, it is typically because a shoe is rubbing up against the lump or when walking or standing barefoot.
Treatment and Prevention
A plantar fibroma will not disappear without treatment, but it can get smaller and be a non-issue. If pain persists, a podiatrist examines the foot and when the arch of the foot is pressed, pain can be felt down to the toes. An MRI or biopsy might be performed to help diagnose or evaluate the plantar fibroma. The following non-surgical options are generally enough to reduce the size and pain of these nodules:
Surgery is considered if the mass increases in size and the patient continues to feel pain after non-surgical methods are tried.
If you have any questions please feel free to contact our office located in York, ME . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.