Blisters are small pockets of fluid that occur on the top layers of the skin for several reasons. Friction, burns, and diseases are all known causes of blisters. Smaller blisters are known as vesicles, while larger blisters are referred to as bulla. The fluid inside the bubble can be blood, pus, or serum; which is a clear liquid that protects the skin. In most cases, blisters are not a major health issue, but they can be an indicator of a more serious condition.
Causes of blisters vary. Blisters are commonly caused by wearing poorly fitted shoes that rub against the foot. However, there are many other causes besides from friction; including burns, sunburn, insect bites, frostbite, poison ivy/oak, chemical exposure, impetigo, eczema, viral infections, and more.
Most blisters heal by themselves and do not require immediate medical care. If you have a blister, do not pop it since this may cause infection; it is advised to put a bandage over the blister to protect it. If the blister is large, causes pain, or if you have a fever, it is recommended that you see a doctor who can provide proper care. Blisters are easy to diagnose, and if considered prudent by the doctor, can easily be drained of fluid with a sterile needle as well.
To prevent blisters on the feet, wear shoes that fit properly and don’t cause rubbing. Socks can help prevent friction and it is recommended that you wear them if you are wearing shoes. Hand blisters can be avoided by wearing gloves during activities that cause friction against the hand. If you have a blister that pops, do not remove the dead skin, wash the area, apply antibiotic ointment, and cover with a bandage. It is okay in most cases to not seek immediate medical care for a blister if it was just caused by friction. However, if the blister causes pain or does not go away, it is suggested that you see a doctor for a diagnosis.

Blood blisters on the foot are caused by friction or trauma that ruptures blood vessels under the skin without breaking the surface. This can occur from wearing ill-fitting shoes, engaging in vigorous activities, or sudden impact injuries. The resulting blister is filled with blood due to the broken capillaries beneath the skin. Blood blisters are generally more painful than regular blisters because of the pressure from the trapped blood. They typically last for about one to two weeks, during which time the body gradually reabsorbs the blood. To aid healing, it is important to protect the blister from further friction or pressure by using padded bandages and avoiding activities that aggravate the area. If you notice you have a blood blister on your foot, it is suggested that you schedule an appointment with a podiatrist who can help you to manage this condition.
Blisters are prone to making everyday activities extremely uncomfortable. If your feet are hurting, contact Dr. Richard DiMario of Maine. Our doctor can provide the care you need to keep you pain-free and on your feet.
Foot Blisters
Foot blisters develop as a result of constantly wearing tight or ill-fitting footwear. This happens due to the constant rubbing from the shoe, which can often lead to pain.
What Are Foot Blisters?
A foot blister is a small fluid-filled pocket that forms on the upper-most layer of the skin. Blisters are filled with clear fluid and can lead to blood drainage or pus if the area becomes infected.
How Do Blisters Form?
Blisters on the feet are often the result of constant friction of skin and material, usually by shoe rubbing. Walking in sandals, boots, or shoes that don’t fit properly for long periods of time can result in a blister. Having consistent foot moisture and humidity can easily lead to blister formation.
Prevention & Treatment
It is important to properly care for the affected area in order to prevent infection and ease the pain. Do not lance the blister and use a Band-Aid to provide pain relief. Also, be sure to keep your feet dry and wear proper fitting shoes. If you see blood or pus in a blister, seek assistance from a podiatrist.
If you have any questions, please feel free to contact our office located in York, ME . We offer the newest diagnostic and treatment technologies for all your foot care needs.

Foot ulcers are open wounds that develop on the feet, often affecting individuals with diabetes or impaired circulation. They typically occur due to a combination of factors, including neuropathy, which is nerve damage, poor blood flow, and pressure from footwear. Foot ulcers can vary in severity, from shallow sores to deep craters, and if left untreated, they can lead to serious complications such as infection and possibly amputation. The primary cause of foot ulcers is prolonged pressure or friction on the skin, which can result from wearing ill-fitting shoes, walking barefoot, or excessive rubbing. In diabetic individuals, high blood sugar levels can further exacerbate the risk by damaging nerves and blood vessels, impairing the body's ability to heal. Other contributing factors may include poor hygiene, smoking, obesity, and a history of foot problems. Recognizing the signs of a foot ulcer, such as redness, swelling, or drainage, is vital for prompt treatment and prevention of complications. If you have a foot wound, it is strongly suggested that you consult a podiatrist who can diagnose its severity, and offer treatment options that are right for you.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Dr. Richard DiMario from Maine. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in York, ME . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.

A bunion, medically termed hallux valgus, is a bony protrusion on the inner side of the foot, precisely at the base of the big toe. This condition arises from the misalignment of the bones in the forefoot, compelling the big toe to angle towards the lesser toes, consequently protruding the joint at its base. Bunions can cause significant discomfort and interfere with your daily activities. If you have exhausted nonsurgical options like padding or orthotic shoes, bunion surgery may be the next step to relieve your pain and improve mobility. During the procedure, a podiatrist may remove the bunion, realign bones, or release tight ligaments to straighten your big toe. Risks of bunion surgery include nerve damage, bone healing issues, or overcorrection. The recovery process often takes up to six months. Initially, you may need to keep your leg elevated to reduce swelling, and it can take weeks before you can comfortably wear regular shoes again. Among the long-term benefits of bunion surgery are improved comfort and mobility. If you are struggling with bunion pain, it is suggested that you consult a podiatrist to discuss whether surgery is right for you.
If you are suffering from bunions, contact Dr. Richard DiMario of Maine. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
If you have any questions, please feel free to contact our office located in York, ME . We offer the newest diagnostic and treatment technologies for all your foot care needs.
A bunion is an enlargement of the base joint of the toe that connects to the foot, often formed from a bony growth or a patch of swollen tissues. It is caused by the inward shifting of the bones in the big toe, toward the other toes of the foot. This shift can cause a serious amount of pain and discomfort. The area around the big toe can become inflamed, red, and painful.
Bunions are most commonly formed in people who are already genetically predisposed to them or other kinds of bone displacements. Existing bunions can be worsened by wearing improperly fitting shoes. Trying to cram your feet into high heels or running or walking in a way that causes too much stress on the feet can exacerbate bunion development. High heels not only push the big toe inward, but shift one's body weight and center of gravity towards the edge of the feet and toes, expediting bone displacement.
A podiatrist knowledgeable in foot structure and biomechanics will be able to quickly diagnose bunions. Bunions must be distinguished from gout or arthritic conditions, so blood tests may be necessary. The podiatrist may order a radiological exam to provide an image of the bone structure. If the x-ray demonstrates an enlargement of the joint near the base of the toe and a shifting toward the smaller toes, this is indicative of a bunion.
Wearing wider shoes can reduce pressure on the bunion and minimize pain, and high heeled shoes should be eliminated for a period of time. This may be enough to eliminate the pain associated with bunions; however, if pain persists, anti-inflammatory drugs may be prescribed. Severe pain may require an injection of steroids near the bunion. Orthotics for shoes may be prescribed which, by altering the pressure on the foot, can be helpful in reducing pain. These do not correct the problem; but by eliminating the pain, they can provide relief.
For cases that do not respond to these methods of treatment, surgery can be done to reposition the toe. A surgeon may do this by taking out a section of bone or by rearranging the ligaments and tendons in the toe to help keep it properly aligned. It may be necessary even after surgery to wear more comfortable shoes that avoid placing pressure on the toe, as the big toe may move back to its former orientation toward the smaller toes.
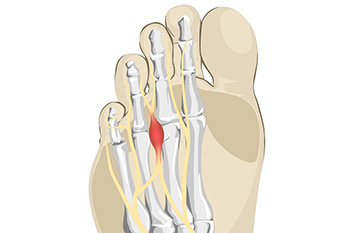
Morton's neuroma, named after the American surgeon Thomas G. Morton who first described it in the 19th century, is a painful condition affecting the nerves in the foot. This benign growth typically forms between the third and fourth toes, resulting from compression or irritation of the interdigital nerve. The exact cause of Morton's neuroma remains elusive, but factors such as wearing tight or high-heeled shoes, engaging in repetitive high-impact activities, or foot deformities may contribute to its development. Symptoms of Morton's neuroma often include a sharp, burning pain or sensation of a lump or foreign object in the ball of the foot. Individuals may also experience numbness, tingling, or a feeling of walking on a pebble. As the condition progresses, discomfort may worsen and become more persistent, particularly during weight-bearing activities. If you have pain in this part of your foot, it may be Morton's neuroma, and it is suggested that you visit a podiatrist. This type of doctor can accurately diagnose and effectively treat this condition.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Dr. Richard DiMario of Maine. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our office located in York, ME . We offer the newest diagnostic and treatment technologies for all your foot care needs.
A neuroma is a thickening of nerve tissue and can develop throughout the body. In the foot, the most common neuroma is a Morton’s neuroma; this typically forms between the third and fourth toes. The thickening of the nerve is typically caused by compression and irritation of the nerve; this thickening can in turn cause enlargement and, in some cases, nerve damage.
Neuromas can be caused by anything that causes compression or irritation of the nerve. A common cause is wearing shoes with tapered toe boxes or high heels that force the toes into the toe boxes. Physical activities that involve repeated pressure to the foot, such as running or basketball, can also create neuromas. Those with foot deformities, such as bunions, hammertoes, or flatfeet, are more likely to develop the condition.
Symptoms of Morton’s neuroma include tingling, burning, numbness, pain, and the feeling that either something is inside the ball of the foot or that something in one’s shoe or sock is bunched up. Symptoms typically begin gradually and can even go away temporarily by removing one’s shoes or massaging the foot. An increase in the intensity of symptoms correlates with the increasing growth of the neuroma.
Treatment for Morton’s neuroma can vary between patients and the severity of the condition. For mild to moderate cases, padding, icing, orthotics, activity modifications, shoe modifications, medications, and injection therapy may be suggested or prescribed. Patients who have not responded successfully to less invasive treatments may require surgery to properly treat their condition. The severity of your condition will determine the procedure performed and the length of recovery afterwards.