
Plantar fasciitis is a common foot condition that gradually develops for various reasons. These can include wearing shoes that do not fit correctly or from gaining weight. Standing on hard or uneven surfaces for most of the day or from recently increasing speed while running can also increase your chance of getting plantar fasciitis. The plantar fascia is found on the bottom of the foot and is the band of tissue that connects the heel to the toes. Any one of the above reasons may cause the plantar fascia to become irritated or torn, and this can lead to plantar fasciitis. Mild relief may be found when specific heel stretches are performed, in addition to wearing shoes that have a cushioned heel. It may help to lose weight if applicable, and elevating the foot frequently may reduce the discomfort. Orthotics may be worn that can provide the necessary support as the foot heals. If you have heel pain, it is suggested that you visit a podiatrist who can treat plantar fasciitis.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Dr. Richard DiMario from Maine. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
How Can It Be Treated?
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our office located in York, ME . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is the thick band of tissue that connects the heel bone to the toes. When this band of connective tissue becomes inflamed, plantar fasciitis occurs. Fortunately, this condition is treatable.
There are several factors that may put you at a greater risk for developing plantar fasciitis. One of the biggest factors is age; plantar fasciitis is common in those between the ages of 40 to 60. People who have jobs that require them to be on their feet are also likely to develop plantar fasciitis. This includes factory workers, teachers, and others who spend a large portion of their day walking around on hard surfaces. Another risk factor is obesity because excess weight can result in extra stress being placed on the plantar fascia.
People with plantar fasciitis often experience a stabbing pain in the heel area. This pain is usually at its worst in the morning, but can also be triggered by periods of standing or sitting. Plantar fasciitis may make it hard to run and walk. It may also make the foot feel stiff and sensitive, which consequently makes walking barefoot difficult.
Treatment for plantar fasciitis depends on the severity of the specific case of the condition. Ice massage applications may be used to reduce pain and inflammation. Physical therapy is often used to treat plantar fasciitis, and this may include stretching exercises. Another treatment option is anti-inflammatory medication, such as ibuprofen.
If you suspect that you have plantar fasciitis, meet with your podiatrist immediately. If left untreated, symptoms may lead to tearing and overstretching of the plantar fascia. The solution is early detection and treatment. Be sure to speak with your podiatrist if you are experiencing heel pain.
Stress fractures are considered to be overuse injuries that are common among runners, as well as other athletes. Football players, basketball players, and dancers are at risk for stress fractures over time. A stress fracture is a hairline crack in the bone as a result of repetitive pounding of the feet. People with poor nutritional habits and who smoke or drink excess alcohol are also susceptible to incurring stress fractures. The most common causes of these painful stress fractures are repetitive force, overtraining, and running on hard surfaces. A stress fracture often develops as the result of a sudden change in physical activity, such as increasing running speed too quickly or starting to participate in a sport after being sedentary for a long time. Furthermore, a vitamin D deficiency can cause the bones to weaken, possibly making them more vulnerable to this type of injury. Wearing shoes that do not fit well or provide inadequate support is another common cause of stress fractures. If you believe you have developed stress fractures in the feet or ankles, it is suggested that you visit a podiatrist for a full examination and correct treatment options.
Stress fractures occur when there is a tiny crack within a bone. To learn more, contact Dr. Richard DiMario from Maine. Our doctor can provide the care you need to keep you pain free and on your feet.
How Are They Caused?
Stress fractures are the result of repetitive force being placed on the bone. Since the lower leg and feet often carry most of the body’s weight, stress fractures are likely to occur in these areas. If you rush into a new exercise, you are more likely to develop a stress fracture since you are starting too much, too soon. Pain resulting from stress fractures may go unnoticed at first, however it may start to worsen over time.
Risk Factors
Stress fractures do not always heal properly, so it is important that you seek help from a podiatrist if you suspect you may have one. Ignoring your stress fracture may cause it to worsen, and you may develop chronic pain as well as additional fractures.
If you have any questions, please feel free to contact our office located in York, ME . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Stress fractures are small breaks in the bone that are caused by repetitive stress. They typically occur due to overuse, forcing the bones of the foot or ankle to continually absorb the full impact of each step taken. Stress fractures can also be caused by abnormal foot structure, osteoporosis, bone deformities, or wearing improper footwear during exercise.
Stress fractures are common for individuals whose daily activities cause high levels of impact on their feet and ankles. Those who run, play tennis or basketball, or practice gymnastics tend to experience these fractures more frequently. Anyone is susceptible to this problem, though. Individuals who are normally sedentary and suddenly begin an intense, high impact workout may sustain stress fractures. This is because their muscles are not yet strong enough to handle and cushion the intensity of their activity. Osteoporosis may also cause someone to get stress fractures, because the disease weakens an afflicted person's bones and makes it easier for them to break down.
Pain from stress fractures typically occurs in the general area of the fracture. Pain can also manifest as “pinpoint pain” or pain that is felt when the site of the injury is touched, and can be accompanied by swelling. It may occur during or after activity, and it may disappear while resting and return when standing or moving. Engaging in any kind of activity, high impact or otherwise, will aggravate the pain. If the intensity of the activity increases before the stress fracture has properly healed, it can cause a full fracture.
Treatment can vary depending on the individual and the degree of injury. The primary way to treat a stress fracture is to rest the hurt foot. Some fractures will heal quickly with only a little bit of rest, while others may require a long rest period and the use of crutches, immobilization, or physical therapy. Under certain circumstances, surgery may be required to install support pins around the fracture to assist in healing.
If you are undergoing a new exercise regimen in running or some other kind of high impact activity, set incremental goals on a weekly basis so you can build up muscle strength. Make sure to wear supportive shoes to better protect you feet.
If you begin to experience any symptoms of stress fractures, you should stop exercising and rest. If the symptoms persist, consult with your podiatrist. Remembering these tips can help you prevent stress fractures to your foot and ankle, and allow you to continue living normally.

Bunions are bony deformities of the big toe joint. They are unattractive, are a common affliction, and can affect people of all ages. Medically, bunions are referred to as hallux valgus. The metatarsal bones in the foot fan out from the base near the ankle to each toe and the distance between them increases as they approach the toes. With bunions, the distance and angle at the base, between the first and second metatarsals, increases over time and a bump develops on a big toe joint. The foot widens and the deformed big toe joint presses uncomfortably against shoes. Pressure from shoes pushes the big toe towards the smaller toes, which emphasizes the bulge on the side of the foot. As time passes, the second toe can lie on top of the big toe and calluses and corns can develop on the toes, leading to further distortion and pain. Walking can also become problematic. If bunions are not tended to, arthritis can develop. It is not just shoes that contribute to bunion formation. Genes, gait, and being female can add to a propensity toward bunions. Wearing narrow-toed shoes or high heels for a prolonged time should be avoided because these types of shoes force the weight down to the ball of the feet and push the toes together. Insoles or orthotics can help and surgery for permanent removal may be an option. If you have a bunion or notice that one may be forming, it is suggested that you consult with a podiatrist who can give you advice and offer treatment options.
If you are suffering from bunions, contact Dr. Richard DiMario of Maine. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
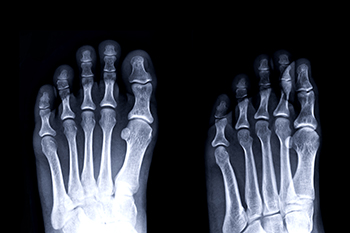
How Are Bunions Diagnosed?
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
If you have any questions, please feel free to contact our office located in York, ME . We offer the newest diagnostic and treatment technologies for all your foot care needs.
A bunion is a bump that forms at the base of the big toe. Bunions form when the big toe pushes against the next toe, which forces the big toe joint to get bigger and stick out. As a result, the skin over the bunion may start to appear red and it may feel sore.
There are risk factors that can increase your chances of developing bunions. People who wear high heels or ill-fitting shoes are more likely to develop them, in addition to those who have a genetic history of bunions or have rheumatoid arthritis.
The most obvious way to tell if you have a bunion is to look for the big toe pushing up against the toe next to it. Bunions produce a large protrusion at the base of the big toe and may or may not cause pain. Other symptoms are redness, swelling, and restricted movement of the big toe if you have arthritis.
Nonsurgical methods are frequently used to treat bunions that aren’t severe. Some methods of nonsurgical treatment are orthotics, icing and resting the foot, taping the foot, and pain medication. Surgery is usually only required in extreme cases. However, if surgery is needed, some procedures may involve removing the swollen tissue from around the big toe joint, straightening the big toe by removing part of the bone, or joining the bones of your affected joint permanently.
Your podiatrist will diagnose your bunion by doing a thorough examination of your foot. He or she may also conduct an x-ray to determine the cause of the bunion and its severity.

A hammertoe occurs when one of the three middle toes bends upward at the middle joint. Corns and calluses that can develop on the hammertoe can make wearing shoes and walking uncomfortable. If lifestyle changes, such as wearing wider shoes, using shoe inserts, or doing stretching and strengthening toe exercises do not help, surgery can be considered to correct a hammertoe. Hammertoe surgery is not a good option for those who have poor circulation in their feet, have a foot infection, or have other health problems making surgery a risk. If considered a good candidate for this surgery, it is typically a procedure that can be done as an outpatient under general anesthesia or using numbing medications. If the hammertoe is still somewhat flexible, a tendon transfer involving redirecting tendons from the bottom of the toe to the top where it is bent can be done to straighten the toe. If the hammertoe is fixed or rigid, a joint resection or fusion can be done. Joint resection is when tendons and ligaments are cut to help straighten the toe and the end of the bone is cut off so the toe can be fully extended. In fusion surgery, the ligaments and tendons are also cut but the two bones forming the affected joint are also cut for straightening the toe. If you have a painful hammertoe, it is suggested that you make an appointment with a podiatrist to see if more conservative treatment is possible or whether surgery is an option for you.
Foot surgery is sometimes necessary to treat a foot ailment. To learn more, contact Dr. Richard DiMario of Maine. Our doctor will assist you with all of your foot and ankle needs.
When Is Surgery Necessary?
Foot and ankle surgery is generally reserved for cases in which less invasive, conservative procedures have failed to alleviate the problem. Some of the cases in which surgery may be necessary include:
What Types of Surgery Are There?
The type of surgery you receive will depend on the nature of the problem you have. Some of the possible surgeries include:
Benefits of Surgery
Although surgery is usually a last resort, it can provide more complete pain relief compared to non-surgical methods and may allow you to finally resume full activity.
Surgical techniques have also become increasingly sophisticated. Techniques like endoscopic surgery allow for smaller incisions and faster recovery times.
If you have any questions please feel free to contact our office located in York, ME . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
In most cases, foot surgery is often chosen as the last available option for conditions that have otherwise been unsuccessfully treated. Surgery may be necessary for several reasons, including the removal of foot deformities (e.g. bone spurs or bunions), arthritis problems, reconstruction due to injury, and congenital malformations (e.g. club foot or flat feet). Regardless of one’s age, foot surgery may be the only successful option for treatment for certain conditions.
The type of surgery one undergoes depends on the type of foot condition the patient has. For the removal of a bunion growth, a bunionectomy is necessary. If the bones in the feet need to be realigned or fused together, a surgical fusion of the foot is needed. For pain or nerve issues, a patient may require surgery in which the tissues surrounding the painful nerve are removed. Initially, less invasive treatments are generally attempted; surgery is often the last measure taken if other treatments are unsuccessful.
While in many cases surgery is often deemed as the final resort, choosing surgery comes with certain benefits. The associated pain experienced in relation to the particular condition is often relieved with surgery, allowing patients to quickly resume daily activities. The greatest benefit, however, is that surgery generally eliminates the problem immediately.
Podiatry history has shown that foot treatments continue to evolve over time. In the field of foot surgery, endoscopic surgery is just one of the many advanced forms of surgery. As technology vastly improves so too will the various techniques in foot surgery, which already require smaller and smaller incisions with the use of better and more efficient tools. Thanks to such innovations, surgery is no longer as invasive as it was in the past, allowing for faster and easier recoveries.