
A sports podiatrist is a healthcare specialist focused on treating and preventing foot and lower limb issues in athletes and other active individuals. They have a deep understanding of how the feet and legs function during physical activities and the specific stresses different sports place on these body parts. The role of a sports podiatrist is vital in enhancing athletic performance and preventing injuries. Sports podiatrists conduct thorough assessments, including gait analysis and biomechanical evaluations, to understand an athlete's foot structure and movement patterns. They offer expert advice on appropriate footwear and can design custom orthotic devices to correct biomechanical imbalances, enhance performance, or prevent injuries. They also treat a range of sports-related foot and ankle problems, ranging from overuse injuries to acute traumas. While all podiatrists can treat sports injuries to some degree, a sports podiatrist offers a more focused expertise in managing and preventing injuries specifically in athletes and those engaged in regular physical activities. If you are an athlete and are experiencing foot or ankle problems, it is suggested that you schedule an appointment with a podiatrist who has experience with sports injuries for an evaluation.
If you are dealing with pain in your feet and ankles, you may want to seek help from a podiatrist. Feel free to contact Dr. Richard DiMario from Maine. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Podiatrist?
A podiatrist is a doctor of podiatric medicine who diagnoses and treats conditions of the foot, ankle, and related structures of the leg. Your podiatrist may specialize in a certain field such as sports medicine, wound care, pediatrics, and diabetic care. Podiatrists have the ability to become board certified through training, clinical experience, and then taking an exam.
What Do Podiatrists Do?
On a daily basis, a podiatrist may perform the following activities:
It is very important that you take care of your feet. It’s easy to take having healthy feet for granted, however foot problems tend to be among the most common health conditions. Podiatrists can help diagnose and treat a variety of feet related conditions, so it is crucial that you visit one if you need assistance.
If you have any questions please feel free to contact our office located in York, ME . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
A podiatrist is a Doctor of Podiatric Medicine who treats the foot, ankle, and related structures of the leg. If you are having any pain, injuries, or abnormalities in these areas, it is best that you seek help from a podiatrist.
Podiatrists complete four years of training in a podiatric medical school. Their training is like that of other physicians, and they may go on to complete a fellowship training after a residency training. Some podiatrists are board certified meaning they have advanced training, clinical experience, and have taken an exam to prove their skills. Certifying boards for podiatry are the American Board of Foot and Ankle Surgery and the American Board of Podiatric Medicine. Podiatrists may work in private practices, hospitals, clinics, or they may even become professors at colleges of podiatric medicine.
While in college, those who want to be podiatrists often take biology, chemistry, and physics classes in preparation for podiatry school. In podiatry school, students study how the bones, nerves, and muscles work together to help you move around. Additionally, they study injuries and how to properly diagnose and treat them. Admittance into podiatric medical school requires the completion of 90 semester hours of undergraduate study with a good grade point average, and acceptable scores on the MCAT (Medical College Admission Test)
Podiatrists treat many different conditions such as: aching feet, ankle pain, bunions, corns, hammertoes, fungus, ingrown toenails, plantar fasciitis, sprains and more. Common forms of treatment for these conditions are physical therapy, drugs, or surgery. Podiatrists may also recommend corrective shoe inserts, custom-made shoes, plaster casts, and strappings to correct deformities.
Even if you are someone whose feet are in generally good condition, you should still visit a podiatrist to have your feet properly exfoliated and maintained, or to make sure you are looking after your feet properly.

Foot blisters are fluid-filled pockets that form on the skin's surface, commonly caused by friction, heat, and moisture. These blisters can be painful and uncomfortable, affecting individuals of all ages. Friction is a primary culprit in blister formation. When the skin repeatedly rubs against footwear or other surfaces, it can lead to irritation, causing a blister to develop as a protective mechanism. Wearing ill-fitting shoes, especially those that are too tight or loose, can exacerbate this problem. Heat and moisture also contribute to blister development. When your feet sweat excessively, it creates a moist environment inside your shoes, increasing the risk of friction. In hot weather, sweat can make the skin more vulnerable to blistering. Another potential cause of blisters is burns, whether from hot surfaces, chemicals, or sunburn, as they can damage the skin and result in blister formation. Understanding the causes of foot blisters is essential for prevention. If you do develop a blister, it is important to protect and care for it to avoid infection and promote healing, and a podiatrist can help you accomplish this. It is suggested that you contact this type of doctor who can guide you toward healing and prevention techniques.
Blisters may appear as a single bubble or in a cluster. They can cause a lot of pain and may be filled with pus, blood, or watery serum. If your feet are hurting, contact Dr. Richard DiMario of Maine. Our doctor can provide the care you need to keep you pain-free and on your feet.
Foot Blisters
Foot blisters are often the result of friction. This happens due to the constant rubbing from shoes, which can lead to pain.
What Are Foot Blisters?
A foot blister is a small fluid-filled pocket that forms on the upper-most layer of the skin. Blisters are filled with clear fluid and can lead to blood drainage or pus if the area becomes infected.
Symptoms
(Blister symptoms may vary depending on what is causing them)
Prevention & Treatment
In order to prevent blisters, you should be sure to wear comfortable shoes with socks that cushion your feet and absorb sweat. Breaking a blister open may increase your chances of developing an infection. However, if your blister breaks, you should wash the area with soap and water immediately and then apply a bandage to the affected area. If your blisters cause severe pain it is important that you call your podiatrist right away.
If you have any questions, please feel free to contact our office located in York, ME . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blisters are a common ailment of people who wear shoes that are either too tight or rub against the feet in an uncomfortable way. Knowing the basics of blisters is important for understanding how they are formed and what treatments should be used for them.
A blister on the foot, or any other part of the body, is a small pocket that is filled with fluid. It usually forms on the upper layer of the skin because these layers are loose enough to allow a blister to form. The most common fluid in a blister is just a clear, watery-like fluid that usually isn’t cause for concern. However, blisters can fill up with blood if they are deep enough and pus if they have become infected with bacteria.
Blisters almost always form on the feet due to shoes rubbing up against the foot, where the friction causes blisters. These can occur after you have walked for a long period of time or when your shoes do not fit you properly. Your feet are also more prone to blisters if they are moist, so keeping them dry and clean is one preventative step you can take.
Preventing infection should be the number one concern when treating blisters, as well as relieving the pain they can cause. Using a bandage to cover up the blister will help it heal and prevent bacteria from entering it. New skin will form under the blister and eventually cause it to pop. You can also take a sterilized pin and try to pop it yourself.
If the blister is filled with pus or blood, seeking treatment from a doctor is ideal. Antibiotics may need to be taken in order to completely eliminate the bacteria inside the blister. See a doctor to have an antibiotic prescribed.
The best way to treat blisters is to prevent them all together. Keeping your feet dry and making sure that your shoes fit properly are just two of the steps you can take to prevent blisters. Shoes that are too tight or shoes that are too loose and allow your feet to slide in them will cause blisters. Applying a bandage to an area where you think a blister is about to form is another way you can prevent them.

Human Papilloma Virus, or HPV, is a large family of viruses, with over 150 types, and it is common for individuals to contract at least one type during their lifetime. Symptoms vary depending on the HPV strain, and while approximately 75 percent of HPV types cause common warts, others lead to more serious conditions. Often, HPV shows no symptoms, making some of its effects silent. For instance, plantar warts are a lesser known manifestation of HPV. They develop under the pressure points of the feet, such as the heels or the balls of the feet, and can be identified by their hard, grainy texture. Although they can be painful due to their location, some individuals may not notice them if they are not causing discomfort. It is advisable to examine your feet regularly, checking for any new growths or changes, including warts, as they could indicate an HPV infection. If you find you have a wart on your foot, it is suggested that you make an appointment with a podiatrist to have it examined and treated as necessary.
Plantar warts can be very uncomfortable. If you need your feet checked, contact Dr. Richard DiMario from Maine. Our doctor will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
Treatment
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact our office located in York, ME . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar warts are growths that typically appear on the heels or other weight-bearing areas of the feet. These warts are caused by the human papillomavirus (HPV). The virus enters the body through breaks in the skin, such as cuts, that are on the bottom of the feet. Plantar warts are more likely to affect children and teenagers, people with weakened immune systems, people who have a history with plantar warts, and people who walk barefoot in environments exposed to a wart-causing virus.
If you suspect you have plantar warts, you may have the following symptoms: pain or tenderness while walking, a lesion that interrupts the ridges in the skin of your foot, small fleshy lesions on the bottom of the foot, or a callus where a wart has grown inward over a well-defined spot on the skin.
HPV causes plantar warts to form and is very common. There are more than 100 kinds of the virus in existence. However, only a few of them cause warts on the feet. The other types of HPV are likely to cause warts on other parts of the body.
If you have plantar warts, your podiatrist may try different treatment methods depending on your specific case. Some treatments for plantar warts are peeling medicines (salicylic acid), freezing medicines (cryotherapy), or surgical procedures. Laser treatments and vaccines are also used to treat plantar warts.
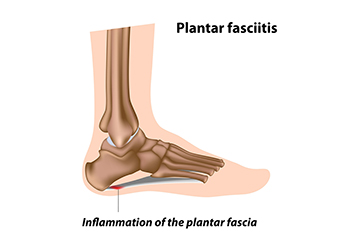
Plantar fasciitis is a common foot condition that results from inflammation and irritation of the plantar fascia, a thick band of tissue connecting the heel bone to the toes. The hallmark symptom of plantar fasciitis is sharp, stabbing heel pain, which can sometimes radiate along the arch or sole of the foot. Some individuals may experience periodic, temporary flares of intense heel pain, while others may have persistent, chronic discomfort in their feet. This pain is often most intense in the morning or after extended rest, and it typically eases within 10 minutes of walking or stretching. However, it can worsen toward the end of the day due to prolonged standing or activities, like climbing stairs and intense exercise, which can stress the plantar fascia. Inflammation of the plantar fascia can lead to visible swelling and redness around the heel and arch of the foot. Even when not visually swollen, the affected area can feel tender and puffy when touched. Additionally, the condition can affect the Achilles tendon, leading to pain. Tightness in the plantar fascia also can cause the foot to roll inward while walking, increasing stress and tension on the Achilles tendon. If you believe you may have plantar fasciitis, it is suggested that you make an appointment with a podiatrist, a medically trained foot doctor, who is able to help you manage this painful condition.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Dr. Richard DiMario from Maine. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our office located in York, ME . We offer the newest diagnostic and treatment technologies for all your foot care needs.
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.